
Video: Meet Chelsea Kirker, Nursing PhD
REDEfine what’s possible in HEALThCARE

Valuable information, insight, and find out what is possible.
Get advice and next steps from a current nursing student.
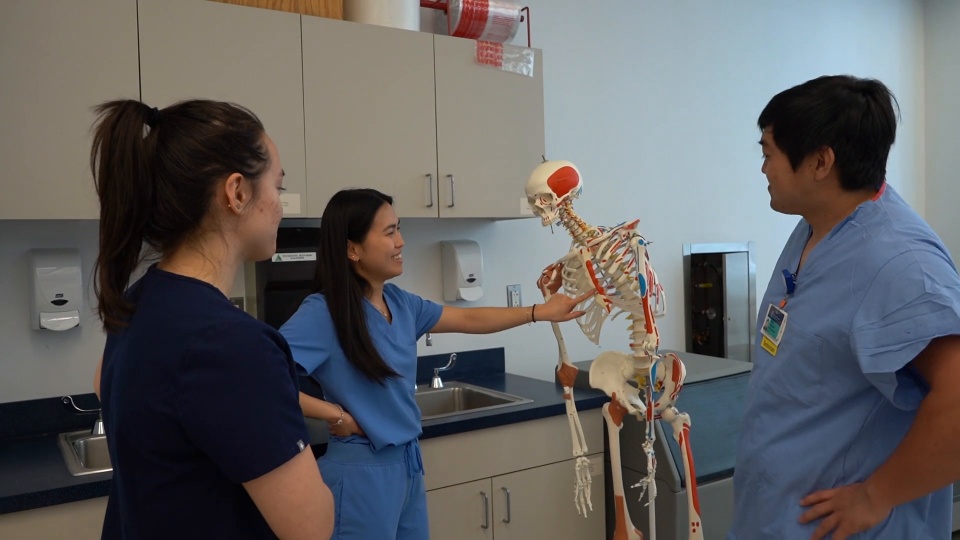
The Bouvé College School of Nursing prepares students through personalized, problem-solving learning experiences in and out of the classroom.
Scientific inquiry meets a caring environment where students become leaders, nurse scientists, educators, advocates, and clinicians – providing equitable and culturally competent healthcare to individual patients, families, communities, and populations locally and globally. Learn why the graduate, undergraduate, and doctorate programs in the School of Nursing are like no other.


Based on our long and rich history of nursing education at Northeastern, we will prepare you for positions of responsibility in all areas of healthcare. Our programs – many offered online – are designed through industry-focused research and collaboration with some of the top hospitals in the world. Our faculty practice in the field; bringing real-world experience and knowledge in the classroom for an education that is unparalleled.

Dr. Choflet joined Bouvé College of Health Sciences in July 2022 as the Assistant Dean for Graduate Nursing Programs and Associate Clinical Professor in the School of Nursing. In addition to her excellent leadership to advance nursing education, her primary research focus is substance use and health improvement strategies for the healthcare workforce and patients.


The mission of Northeastern University School of Nursing is to educate students to provide evidence-based, culturally and linguistically competent, ethical healthcare that is high quality, safe, accessible to diverse local, national, and global communities. Our programs prepare students to become leaders as nurse clinicians, educators, scholars, and researchers.

The mission of the School of Nursing is to make significant contributions to health and the discipline of nursing by advancing science, demonstration leadership and innovation in practice excellence, and embracing the values of diversity, inclusion, and equity.
The School of Nursing provides a caring environment to foster scientific inquiry and prepare students to become leaders, nurse scientists, educators, advocates, and clinicians to provide equitable and culturally competent healthcare to individual patients, families, communities and populations locally and globally.

Strategic Goal #1
Become a leader in generating scholarship for academic nursing-scholarship of discovery, practice and teaching
Position the SON for excellence by enhancing a supportive and nurturing culture for the creation of scholarship.
Strategic Goal #2
Provide students with dynamic experiential learning opportunities across the curriculum, including clinical and research practica, Co-op experiences and community partnerships, locally and globally.
Enhance existing experiential student learning opportunities locally and globally.
Nurturing existing & expand new partnerships with leaders from communities, government, industry and non-profit organizations.
Strategic Goal #3
Promote opportunities for students, faculty, and academic support staff to engage in entrepreneurial and innovative projects, especially those that foster interprofessional collaboration.
Expand opportunities that foster innovation & collaboration across campus and/or with community entities.
Create and launch a SON publication to feature SON innovations, achievement and contributions to advancing health; diversity initiatives to be disseminated on campus, to alumni and available on-line.
Strategic Goal #4
Enhance our efforts and capacity for recruiting, educating, retaining and supporting a diverse and talented community
Increase number of faculty from under-represented minorities (URM) and men.
Create and launch a SON publication to feature SON innovations, achievement and contributions to advancing health; diversity initiatives to be disseminated on campus, to alumni and available on-line.
Strengthen the synergy among all members of SoN community towards a healthy work environment.
Strategic Goal #5
Strategically grow and strengthen our educational programs and scholarship to reflect the global healthcare needs of individual patients, families, communities, and populations
Enrich and contemporize existing education programs through discovery and innovation.
Enhance experiential learning in global health locally and abroad.
At Northeastern University, we create the conditions for robust, deep and flexible learning that will prepare our students for a life of fulfillment and accomplishment in a world that is continually changing. While learning happens in classroom, lab and studio situations, it is much more powerful and robust when students have opportunities to use their knowledge and practice their skills in authentic, real-world situations. Below are listed the expected learning outcomes for our nursing students by program.
Download the Program Learning Outcomes [PDF]
Leadership
Apply leadership concepts and skills in the provision of patient-centered care while promoting social justice, health, and wellness.
Scientific Inquiry
Demonstrate clinical judgment based on the best evidence in achieving high quality patient outcomes.
Practice Excellence (Scholarship)
Integrate best evidence, clinical expertise and patient values and preferences in the implementation of patient-centered care, and health promotion and wellness.
Quality Care
Provide high quality patient-centered care through application of practice improvements to create a safe environment for care delivery.
Diversity, Equity, and Inclusion
Deliver culturally appropriate (or culturally competent) patient centered care for equity and inclusion to all populations.
Innovation
Use patient care technology, information systems, and communication devices to provide patient-centered care.
Interdisciplinary Collaboration
Collaborate effectively with individuals, families, interdisciplinary teams in delivery of quality patient care.
Practice Excellence (Systems)
Identify institutional/community system resources to provide safe, effective and equitable healthcare to individuals and diverse populations.
Leadership
Lead change to advance healthcare for individuals and communities while promoting and advocating for human rights, equity, and self-care.
Scientific Inquiry
Uses expert clinical reasoning to assess, intervene, and evaluate the outcomes of interventions with patients, families, communities, and systems of care.
Practice Excellence (Scholarship)
Implements and evaluates, translates best available evidence into clinical practice for the promotion of health and wellness.
Quality Care
Evaluate patient-centered care systems and clinical outcomes in order to implement strategies to reduce risk and improve the quality of care.
Diversity, Equity, and Inclusion
Create environments that promote culturally competent care for equity and inclusion to all populations, while promoting and advocation for human rights and equity.
Interdisciplinary Collaboration
Partners with colleagues across multiple professions to meet healthcare needs of patients, families, communities, and systems of care.
Innovation
Maximize use of health information technology to communicate among providers, consumers, government agencies and insurers.
Practice Excellence (Systems)
Participates in institutional/community system wide initiatives that improve clinical or educational outcomes and promotes equity and inclusion of individuals and diverse populations.
Leadership
Leads the design, implementation, evaluation, and dissemination of evidence-based practice improvement initiatives while promoting policies that advance health, social justice, and equity.
Scientific Enquiry
Critically analyzes complex clinical situations and practice environments to catalyze change in health care system.
Practice Excellence (Scholarhip)
Translate evidence to develop new models for nursing practice that will transform healthcare and promote health and wellness.
Quality Care
Direct the development and implementation of social, economic, political and health policy to ensure quality and safety of health care delivery.
Diversity, Equity, and Inclusion
Establish and evaluate cultural competency initiatives to promote equity and inclusion in healthcare and health outcomes.
Interdisciplinary Collaboration
Lead and diffuse interdisciplinary care coordination teams and collaborative efforts. (IOM, 2003)
Innovation
Evaluate and analyze the impact of health information technology implementation on organizations and nursing practice.
Practice Excellence (Systems)
Leads and coordinates resources within an institutional/community system to promote patient-centered, safe and effective, and equitable care to diverse populations.
Leadership
Leads the design, implementation, evaluation, and dissemination of evidence-based practice improvement initiatives while promoting policies that advance health, social justice, and equity.
Scientific Inquiry
Critically analyzes complex clinical situations and practice environments to catalyze change in health care system.
Practice Excellence
Translate evidence to develop new models for nursing practice that will transform health care.
Quality Care
Direct the development and implementation of social, economic, political and health policy to ensure quality of health care.
Diversity, Equity, and Inclusion
Establish and evaluate cultural competency initiatives to promote equity and inclusion in healthcare and health outcomes.
Interdisciplinary Collaboration
Lead and diffuse interdisciplinary care coordination teams and collaborative efforts.(IOM, 2003)
Innovation
Evaluate and analyze the impact of health information technology implementation on organizations and nursing practice.
Students will be able to:
Northeastern University has maintained its status as a member in good standing of the New England Commission of Higher Education, Inc. (NECHE), previously New England Association of Schools and Colleges (NEASC), since it was awarded its initial accreditation in 1940. The university was last reviewed by NECHE in 2018 and will be reviewed again in fall 2028.
Northeastern University possesses degree-granting authority in Massachusetts, under the auspices of the Massachusetts Board of Higher Education.
The prelicensure programs at Northeastern University School of Nursing Boston campus are approved by the Massachusetts Board of Registration in Nursing.
The prelicensure program at Northeastern University School of Nursing, Charlotte campus is approved by the North Carolina Board of Nursing.

The Baccalaureate, Master’s and Doctor of Nursing Practice programs at Northeastern University School of Nursing are accredited by the Commission on Collegiate Nursing Education, 655 K Street, NW, Suite 750, Washington, DC 20001, 202-887-6791

Northeastern University School of Nursing is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center’s Commission on Accreditation.

Northeastern University is accredited by the the International Federation of Nurse Anesthetists (IFNA).
102 Robinson Hall
360 Huntington Ave
Boston, MA 02115
Tel: 617-373-3649
Fax: 617-373-8675
General Admissions
617-373-2200
External Transfer Admissions
617-373-2200
Admissions Visitor Center
617-373-4097
Program Office
617-373-6083
Accelerated Bachelor of Science in Nursing (ABSN)
1-888-892-3819
Doctor of Nursing Practice
Lynn Reede
[email protected]
Doctor of Nursing Practice — Nurse Anesthesia
Connie Lorette
[email protected]
617-373-3124
Doctor of Philosophy
Jane Saczynski
[email protected]
617-373-2521
We welcome any questions you might have about our programs. Please feel free to send us general program inquiries and admissions-related questions to:
[email protected]
Direct Entry Nursing (MS)
Lauren Spendley
[email protected]
617-373-7055
Family Nurse Practitioner
Mary Lynn Fahey
[email protected]
Adult-Gerontology Acute Care Nurse Practitioner
Stephen Wood
[email protected]
Adult-Gerontology Primary Care Nurse Practitioner
Carol Patton
[email protected]
Neonatal Nurse Practitioner
Acute Care/Primary Care
Gretchen Hamn
[email protected]
Pediatric Nurse Practitioner
Acute Care/Primary Care
Marketa Rejtar
[email protected]
Psychiatric Mental Health Nurse Practitioner
Ann Polcari
[email protected]
Graduate Certificate in Patient Safety
Halima Mastawi
[email protected]