Health outcomes research plays a key role in promoting a patient’s quality of life and has become increasingly popular for healthcare professionals working to improve the quality of care. It reveals the value of health data through large-scale analytics, showing what works for whom and at what cost.
Read on to learn about the importance of health outcomes research and its connection to real-world evidence.
What are health outcomes?
Health outcomes are changes in health as a result of a specific healthcare intervention.
According to Kristin Kostka, director of the OHDSI Center at Northeastern University’s Roux Institute, “Anything that happened to you that describes your health state could be considered a potential health outcome.”
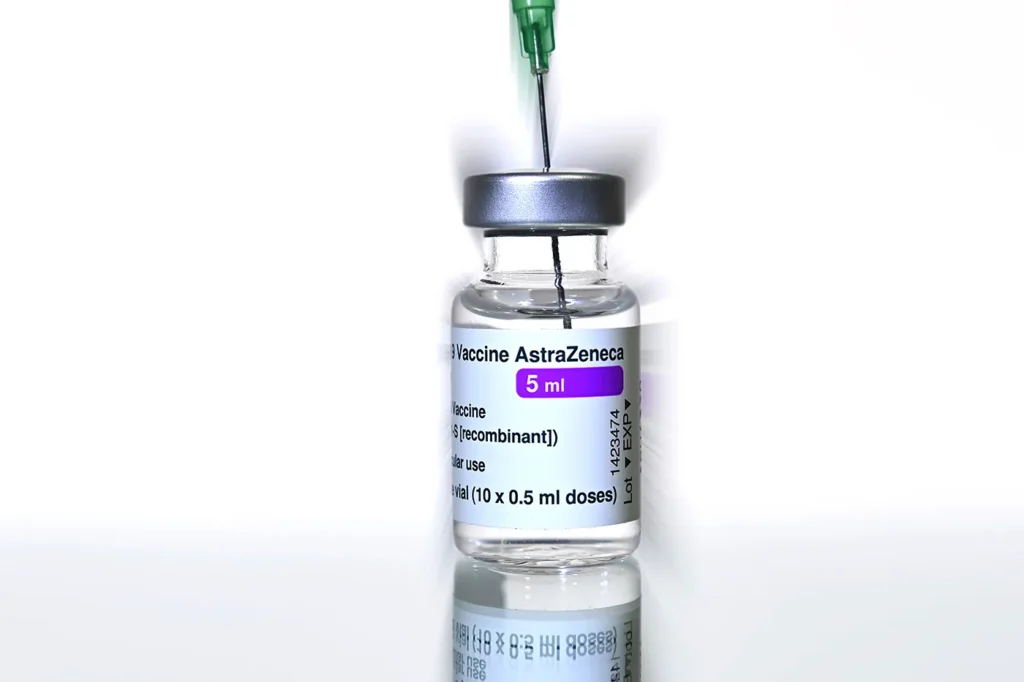
For instance, will getting the Johnson & Johnson one-dose vaccine keep me from getting severe COVID, or will diet and exercise help me live longer? These are examples of health outcomes.
What is health outcomes research?
Health outcomes research, sometimes called health economics or outcomes research, is the methodology used to measure the results of various healthcare interventions. Simply put, it helps determine what works and what doesn’t. The objective of health outcomes research is to improve health-related quality of life.
Health outcomes research can come from a variety of sources:
- Clinical observations from clinical trials
- Patient-reported outcomes from patients’ own observations and experiences
- Financial impacts of what the financial outcomes are
- Measurable data, such as mortality rates and other measurable outcomes
Why is health outcomes research important?
Health outcomes research is an important part of working to prevent adverse medical events and reduce a patient’s risk of harm.
“A lot of the time we’re reactive, but good, systematic, large-scale health outcomes research is the framework for how we improve health outcomes overall,” Kostka says.
The data collected allows both researchers and consumers to have good information to work with regarding the best quality of care.
Health outcomes research and real-world evidence
So how does health outcomes research connect to real-world evidence? According to the U.S. Food and Drug Administration (FDA), real-world evidence (RWE) is the culmination of clinical evidence regarding the usage and potential benefits or risks of a procedure or medical product derived from analysis of real-world data. Health outcomes research and RWE work together by turning the data into evidence.
“It’s the rigor and process by which health outcomes researchers take information generated by patients or in their routine healthcare services and turn that into a rigorously validated piece of information that can be used for decision making,” Kostka notes.
Kostka explains that doesn’t mean health outcomes research doesn’t inform decision making, but generally, RWE indicates that something can pass a regulatory grade assessment, which is a stringent bar. For example, in the context of therapies on market: are they working, not working; is it safe, not safe?
Health outcomes researchers could be looking at a whole number of other things like disability research or social determinants of health. While not all of these get turned into evidence, they’re still important to know.
Is a career in health outcomes research for you?
Now that you’ve learned more about health outcomes research and how it relates to real-world evidence, are you interested in becoming a health outcomes researcher? If so, Northeastern can help.
Most health outcomes researcher jobs—roughly 66 percent—require at least a master’s degree. If you’re ready to get started in this exciting field, consider Northeastern’s Master of Science in Real-World Evidence in Healthcare and Life Sciences.
Download Our Free Guide

Career Guide
Learn how to advance your real-world evidence career.