research applied


Video: Learn about Health Equity and Social Justice Research in Action
Disparities in health and mental health arise and persist as the result of complex individual, societal, and global factors. We bring together faculty and students from across Northeastern University, along with external research partners, to tackle these complex challenges. Our teams draw upon a wide range of research methods and interventions, but share a common commitment to promoting health equity and social justice through high-impact, community engaged research.


REAL-WORLD

research area
For more than a decade, the institute has organized interdisciplinary research teams to improve the lives of refugee and immigrant populations. We work with partners such as Harvard Medical School and Boston Children’s Hospital to explore discrimination and health issues among Somali refugees. Another current project involves the impact that sanctuary cities have on health and well-being have on its communities.
world class

research area
The institute conducts research on the cause and prevention of violence, including child abuse, youth violence, sexual assault, community violence, and intimate partner/teen dating violence. We evaluate the effectiveness of proposed interventions and develop new interventions based on an ecological approach to environmental, social, and individual determinants of violence.
thought leaders

research area
The institute is home to national thought leaders in behavioral health research, with a special emphasis on mental health and substance abuse. We explore how stigma, discrimination, and socioeconomic factors affect access to education, employment, and medical health. The institute also promotes public involvement in our research through community-based participatory research methods.
community

research area
Institute faculty research how social and economic factors influence health and disease prevention. Currently, we are focused on HIV/AIDS, obesity, and Hepatitis C, as well as how racial and ethnic disparities affect pregnancy outcomes across generations.
Health Equity Interns are Northeastern University undergraduate students who commit to working four hours a week during one academic semester at the Institute on Health Equity and Social Justice Research in its mission of conducting research towards advancing health equity and social inclusion and reducing health disparities. Opportunities are available for interns to continue an affiliation with the Institute once the semester internship is completed.
APPLICATION NOW OPEN!
The health equity internship includes the following:
Your responsibilities would be as follows:
The Fall 2024 Health Equity Internship application is open until Sunday, April 21st.
Please reach out to Suzanne Garverich at [email protected] with any questions regarding the application process.
*Please note that first semester Health Equity Interns must be enrolled in classes and cannot be on co-op.*
Starting in the spring of 2022 we will have an opportunity for a dual internship experience with the Women’s Research and Engagement Network (WREN). WREN, is a student-led program dedicated to promoting and celebrating the success of female-aligned individuals at Northeastern.
As a dual program member, you will receive all the benefits of the Health Equity Internship program and more. You will be considered a WREN Scholar, meaning that you will have access to career panels, skills-based trainings, and social networking nights with an interdisciplinary cohort of undergraduate women in research.
During fall semesters, Scholars also will be eligible to present their research at the WREN Summit, the nation’s first undergraduate interdisciplinary women’s research conference.
To support your participation in both the WREN Scholar Program and the Health Equity Internship, attendance requirements for each will be adjusted accordingly. There will be an additional 2-3 hours of events/trainings a month for the dual internship.
If you are a female-aligned individual and would like to apply to the dual internship please indicate that on the Health Equity Intern application.
With the support the Bouvé College of Health Sciences, the Institute for Health Equity and Social Justice Research has been able to provide funding to support Faculty Scholars as they develop their research portfolios in advancing the goals of health equity for diverse populations made vulnerable through marginalization and exclusion through the Advancing Health Equity Pilot Awards.
The PEAK Experiences Awards are funded by the Office of Undergraduate Research and Fellowships, a progressively structured sequence of opportunities designed to support students as they continue climbing to new heights of achievement in undergraduate research and creative endeavor throughout their Northeastern journeys.

Rachel Rodgers
Associate Professor
Bouvé College of Health Sciences
Title: Towards Parent-led Interventions for Body Inclusiveness

Dani Snyder-Young
Assistant Professor
College of Arts, Media and Design
Title: Studying Social Stigma and Affect in Diverse Audiences of “This is Treatment”

Danielle Crookes
Assistant Professor
Bouvé College of Health Sciences & College of Social Science and Humanities
Title: Sanctuary Policies and Receipt of Preventive Cardiovascular Care Among Immigrants in the US

John Olawepo
Assistant Teaching Professor
Bouvé College of Health Sciences
Title: An Exploration of Barriers to and Facilitators of Sickle Cell Disease Newborn Screening in Nigeria: A Qualitative Study

Leanne Chukoskie
Associate Professor
Bouvé College of Health Sciences & College of Arts, Media and Design
Title: An Intergenerational Game Jam

Rebekah Moore
Assistant Professor
College of Arts, Media and Design
Title: Advancing Racial and Health Equity through the Arts: A community-engaged research study in the city of Boston

Lorna Hayward
Associate Professor
Bouvé College of Health Sciences
Title: Increasing Access to Equitable Adaptive Sports Opportunities to Promote Physical and Mental Health for College Students with Disabilities

Amy Lu
Associate Professor
College of Arts, Media and Design aBouvé College of Health Sciences
Title: How effective are active video games? A meta-analysis across the lifespan in clinical and nonclinical populations

Linda Blum
Professor of Sociology
College of Social Sciences and Humanities
Title: BRCA Communities In the Pandemic: Exploring the Role of Online Peer Support

Collette Ncube
Research Associate of Epidemiology
Boston University School of Public Health
Title: Un-Masking the Origins of Maternal Mortality/Morbidity Inequities (UMOMMI)

Danielle Levac
Assistant Professor
Bouvé College of Health Sciences
Title: Immersive virtual reality as a training modality for the development of a growth mindset in economically-disadvantaged children and youth

Hermine Poghosyan
Assistant Professor
Faculty, School of Nursing
Title: Racial/ethnic disparities in lung cancer screening potentially due to current screening guidelines

Tiffany Joseph
Associate Professor
College of Social Science and Humanities
Title: (Not) All In: Race, Ethnicity, Immigration, Exclusion, and Health Care in America’s City on a Hill

Dami Ko
Assistant Professor
School of Nursing
Title: Socioeconomic Inequities in Health among Urban Liver Transplant Recipients

Miso Kim
Assistant Professor
College of Arts, Media and Design
Title: Designing services to assist isolated older adults in senior living centers during COVID-19

Kara Pavone
Assistant Professor
Bouvé College of Health Sciences
Title: Pain-Related Disparities Among Patients with Substance Use Disorder

Rachel Rodgers
Associate Professor
College of Social Sciences and Humanities and Bouvé College of Health Sciences
Title: Beyond White Bread: A Delphi Study for an Equitable Healthy Eating Scale

Margo Lindauer
Associate Professor
School of Law and Bouvé College of Health Sciences
Project: Domestic Violence Clinic

Julia Zalvino, COS ’24
College of Arts, Media and Design
Title: “Which Types of Social Media Are Helpful for Body Image: Hearing from Diverse Youth”
Mentor: Professor Rachel Rodgers, Department of Applied Psychology, Bouvé
Base Camp Award

Haley Moriarty, Bouvé ’23
Title: “Parenting in the Time of Social Media: A Qualitative Study of Parental Involvement in Teens’ Social Media Use”
Mentor: Professor Rachel Rodgers, Department of Psychology, Bouvé
Base Camp Award

Julia Dierker, Bouvé ’24
Title: “Mixed-Method Telehealth Research”
Mentor: Professor Dami Ko, School of Nursing, Bouvé
Base Camp Award

Julia Denlinger, Bouvé ’22
Title: “Firearm Suicide Prevention Strategies for Firearm Owners and the Preventability of Firearm Suicide”
Mentor: Suzanne Garverich, Institute for Health Equity & Social Justice Research, Bouvé
Base Camp Award

Meghna Iyer, Bouvé ’22
Title: “Improving Guardrail Damage Reporting to Promote Injury Prevention in Motor Vehicle Crashes”
Mentor: Professor Alisa Lincoln, Department of Health Sciences, Bouvé
Summit Award

Jasper Duval, CSSH ’23
Title: “‘Pray to the Mumbai Government’: Government Officials and Legal Exclusion in a Non-notified Settlement in India”
Mentor: Professor Liza Weinstein, Department of Sociology and Anthropology, CSSH
Summit Award

Owen Graham-O’Regan, CSSH ’23
Title: “Changing Laws or Changing Norms? The Impact of Female Leadership on Intimate Partner Violence in India”
Mentor: Professor Bilge Erten, Department of Economics, CSSH
Ascent Award

Dorian Stump, Bouvé ’22
Title: “American Firearm Suicide Prevention Project”
Mentor: Professor Alisa Lincoln, Department of Health Sciences, Bouvé
Base Camp Award

Rayna Haque, Bouvé ’22
Title: “Somali Parent Perspectives on Barriers to Diagnosis in Children with Developmental Disabilities”
Mentor: Carmel Salhi, Bouvé, Health Sciences
Summit Award

Summer Kelly Bouvé ’24
Title: “Un-Masking the Origins of Maternal Mortality/Morbidity Inequities: Measurement and Determinants of Racial/Ethnic Disparities in Severe Maternal Morbidity”
Mentor: Alisa Lincoln, Bouvé, Health Sciences
Ascent Award

Julia Denlinger Bouvé’22
Title: “Firearm Suicide Prevention Project”
Mentor: Alisa Lincoln, Bouvé, Health Sciences
Ascent Award

Dorian Stump Bouvé ’22
Title: “Firearm Suicide Prevention Project”
Mentors: Suzanne Garverich, Institute for Health Equity and Social Justice Research; and Alisa Lincoln, Bouvé, Health Sciences
Ascent Award

Sara Lowell COS ’24
Title: “Identification of Areas for Improved Alignment in the Human Services Sector with State Government Entities”
Mentors: Amy Helburn, Bouvé, Health Sciences
Ascent Award

Olivia Durant Bouvé ’23
Title: “The Lived Experience of Calciphylaxis: Living with a Disease of Clinically Uncertain Etiology”
Mentors: Carmel Salhi, Bouvé, Health Sciences
Trail-Blazer Award

Valeria Do Vale, CSSH ’21
Title: “Immigrants’ Healthcare Access Under Shifting Public Policies”
Mentor: Professor Tiffany Joseph, Sociology and Anthropology
Ascent Award

Maya Rabow, COS ’23
Title: “Crisis Responses in Early Childhood Mental Health during COVID-19: The Importance of Systems-Building”
Mentor: Professor Beth Molnar, Health Sciences
Base Camp Award

Angelica Fuiza, Bouvé ’22
Title: “Twenty Seconds a Day: The Impact of Tiktok Diet Culture Content on Young Women”
Mentor: Professor Rachel Rodgers, Applied Psychology
Summit Award

Jasper Duval, CSSH ’23
Title: “The Shame of the Slum: An Exploratory Study of Territorial Stigma and Mental Wellbeing in a Non-Notified Settlement in Mumbai”
Mentor: Professor Liza Weinstein, Sociology and Anthropology
Ascent Award

Kevin Dunne, CSSH ’21
Title: “COVID-19 and Domestic Violence”
Mentor: Professor Bilge Erten, Economics
Base Camp Award

Anisa Amiji, Bouvé ’22
Title: “Examining Information-Seeking During COVID-19”
Mentor: Professor Miso Kim, Art + Design
Base Camp Award

Cate Henning, Bouvé ’23
Title: “Drug-Induced Homicides: The Solution or the Problem?”
Mentor: Professor Leo Beletsky, Health Sciences
Base Camp Award

Gal Nissan, Bouvé ’22
Title: “The Longitudinal Effects of Body Image Concerns on Health Outcomes”
Mentor: Professor Rachel Rodgers, Psychology
Base Camp Award

Cullen Bober, Bouvé ’21
Title: “Exploring DIH Charges and Carceral Budgets”
Mentor: Professor Leo Beletsky, Health Sciences
Ascent Award

Meghna Iyer, Bouvé ’22
Title: “Improving Guardrail Damage Reporting to Promote Injury Prevention in Motor Vehicle Accidents”
Mentor: Professor Alisa Lincoln, Health Sciences
Summit Award

Kenadi Kaewmanaprasert, Bouvé ’24
Title: “Influence of Documentation Status and Race on Immigrant Healthcare Access”
Mentor: Professor Tiffany Joseph, Sociology and Anthropology
Ascent Award

Rayna Haque, Bouvé ’22
Title: “A Qualitative Review of Mental Health and Exposure to Violence in Resettled Refugees”
Mentor: Professor Carmel Salhi, Health Sciences
Ascent Award

Shurobhi Nandi, COS ’22
Title: “Improving Access to Early Childhood Mental Health Services in Child Welfare”
Mentor: Professor Beth Molnar, Health Sciences
Ascent Award

Winnie Li, Bouvé ’21
Title: “Digital Media Use and Mental Health in College Students”
Mentor: Professor Lichuan Ye, Nursing
Ascent Award

Jasper Duval, CSSH ’23
Title: “The Shame of the Slum: An Exploratory Study of Territorial Stigma and Mental Well-Being in a Non-Notified Settlement in Mumbai”
Mentor: Professor Liza Weinstein, Sociology and Anthropology
Ascent Award

Connor Holmes, Bouvé ’21
Title: “Exploring Transgender, Non-binary, and Genderqueer Dating App Use”
Mentor: Professor Laura Senier, Health Sciences
Summit Award

Lujane Barakat, Bouvé ’21
Title: “Oral Health Behaviors and Self-Image”
Mentor: Professor Rachel Rodgers, Applied Psychology
Ascent Award

Yechan Yang, COS ’22
Title: “LGBTQ Health Care Disparities in Telemedicine”
Mentor: Professor Alisa Lincoln, Bouvé College of Health Sciences, Health Sciences
Base Camp Award

Morgan Wong, Bouvé ’24
Title: “Un-Masking the Origins of Maternal Mortality/Morbidity Inequities (UMOMMI)”
Mentor: Professor Collette Ncube, Bouvé College of Health Sciences, Health Sciences
Base Camp Award

Ciara Sosnowski, CAMD ’23
Title: “Arts, Health, and Wellbeing: A Literature Review”
Mentor: Professor Rebekah Moore, CAMD, Music
Summit Award
Thao-Mi Nguyen, Bouvé ’25
Title: “Un-Masking the Origins of Maternal Mortality/Morbidity Inequities (UMOMMI)”
Mentor: Professor Collette Ncube, Bouvé College of Health Sciences, Health Sciences
Base Camp Award

Nikita Murli, COS ’23
Title: “Tracking Drug-Induced Homicide (DIH) Charges in the United States”
Mentor: Professor Leo Beletsky, Bouvé College of Health Sciences, Law and Public Policy
Base Camp Award

Jasper Duval, CSSH ’23
Title: “‘We Live in Garbage’: Legal Exclusion in a Non-Notified Settlement in Mumbai”
Mentor: Professor Liza Weinstein, CSSH, Sociology and Anthropology
Summit Award

Kevin Dunne, CSSH ’22
Title: “COVID-19 and Mental Health”
Mentor: Professor Bilge Erten, CSSH, Economics
Ascent Award
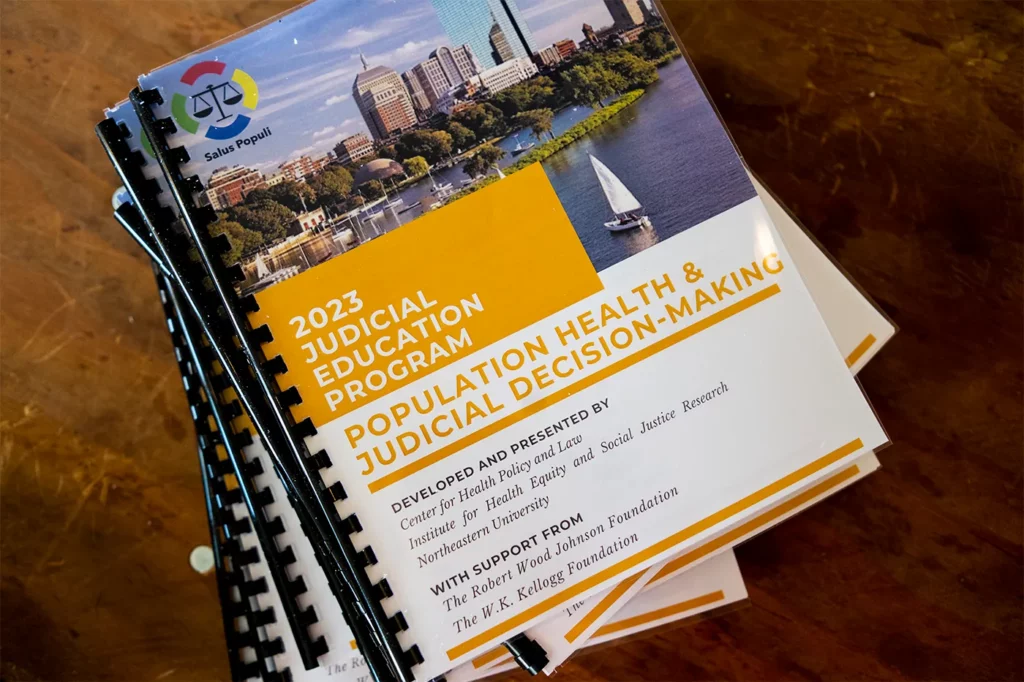
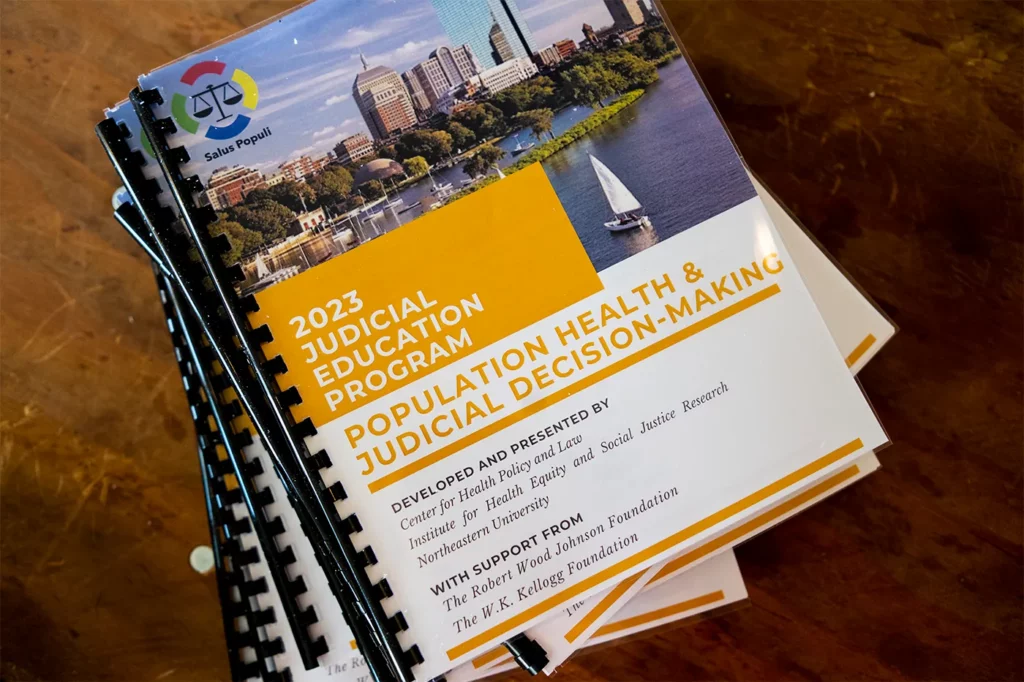
This has been an exciting and productive year for us at the Institute for Health Equity and Social Justice Research. As you will see in the reports our teams of faculty, students, and community partners have been busy with new and exciting programmatic and research efforts.
The mission of this institute is to generate scientific knowledge needed to promote health equity and social justice, and reduce disparities in health, mental health, and well-being.
The Institute on Urban Health Research was first funded in 2001 as part of Provost’s initiative and was led by its Founding Director, Dr. Hortensia Amaro. The IUHR was formed as a university-wide research center that would engage faculty and students from diverse disciplines. It later was moved into Bouvé College of Health Sciences, which remains our home college.
Later the Institute name was amended to The Institute on Urban Health Research and Practice under the leadership of John Auerbach. In 2018, with the appointment of Dr. Alisa K. Lincoln as the Institute Director, we have changed our name and are now the Institute for Health Equity and Social Justice Research.
The Institute remains committed to the core mission first established in 2001 to improve the health and well-being of the residents of Boston and other urban communities. The Institute is focused on the social determinants of health in urban settings, the promotion of health equity and the elimination of health disparities. However, with the growth of the Institute, our ongoing work with diverse groups of students, faculty and community partners, and the current scientific and social needs, we have rearticulated our mission to include greater attention to health equity and social justice and to reflect our partnerships with the growing number of communities impacted by inequity and social marginalization.
Despite tremendous advances in health care, the benefits of these advances have not been equally shared across communities. Many communities experience disparities in health, mental health, and well-being and at the Institute for Health Equity and Social Justice Research our teams of interdisciplinary researchers, students and community partners are engaged in a wide-range of efforts to prevent and reduce these health disparities associated with race, gender, neighborhood, immigration status, sexual orientation, and other stigmatized or marginalized statuses.
We focus attention on the social and economic determinants of health and mental health and increasing understanding of the factors that challenge health and well-being and those that promote community strength and resilience. Our teams are engaged in the development of strategies to reduce disparities through intervention and policy aimed at promoting health equity and social justice.
Disparities in health and mental health arise and persist as the result of complex individual, community, societal and global factors. At the Institute for Health Equity and Social Justice Research we bring together faculty and students from across Northeastern University’s many departments and colleges, along with our research partners, to tackle these complex challenges. Our teams draw upon a wide range of research methods and intervention strategies but share common commitments to promoting health equity and social justice through high-impact, community engaged research.
To learn more about what we do, or for more information on how to work with the Institute of Health Equity and Social Justice Research (IHESJR), contact us.
Phone: 617-373-5813
Hours: 9:00AM – 5:00PM (ET)
Postal Address:
Northeastern University
360 Huntington Ave, 314 INV
Boston, MA 02115
For questions related to the Vicarious Trauma Toolkit, please email Vicarious Trauma Toolkit Information.